The Hidden Universe Inside You: How Gut Bacteria Influence Your Mind
That persistent brain fog? Those unpredictable mood swings? Your child’s inability to focus? The trillions of microorganisms inhabiting your gut might be the puppet masters.
For decades, we’ve examined the brain in isolation, treating it with medications to correct chemical imbalances while overlooking what might be the true command center: the vast microbial ecosystem thriving in your intestines.
TL;DR:
- Your gut is teeming with 100 trillion bacteria - 10× more than your human cells, producing neurotransmitters that affect mood and cognition
- Schizophrenia has a bacterial signature - Specific gut bacteria patterns can predict diagnosis, and transplanting these bacteria into mice induces schizophrenia-like symptoms
- ADHD linked to gut dysbiosis - Distinct microbiome patterns, disrupted dopamine production, and early antibiotic use increasing ADHD risk by 40%
- The gut-brain communication highway - Vagus nerve signaling, microbial neurotransmitter factories (90% of serotonin made in gut), and inflammation connection
- Cutting-edge treatments emerging - Fecal transplants showing promise for mental health, precision bacterial formulations targeting specific conditions
- Practical strategies to optimize your microbiome - 30 plant challenge, fiber diversity, fermented foods, eliminating ultra-processed foods, rethinking antibiotics, breaking stress-gut cycle
Your Second Brain Is Teeming With Microbes
Your intestinal tract contains:
- 100 TRILLION bacteria (vastly outnumbering your own cells)
- Over 1,000 different species with unique functions
- 3 MILLION bacterial genes (compared to your mere 25,000 human genes)
- 70-80% of your entire immune system
This isn’t just random microbial hitchhikers. It’s a sophisticated ecosystem that influences everything from digestion to brain function. When this delicate balance gets disrupted, both physical and mental health can deteriorate rapidly.
The Schizophrenia Connection: A Paradigm Shift
For generations, we’ve approached schizophrenia as primarily a brain disorder, relying on antipsychotics that target dopamine receptors. But what if we’ve been focusing on the wrong end of the body?
✅ The “Schizophrenia Signature” in Gut Bacteria
A groundbreaking 2019 study in Science Advances discovered something remarkable: people with schizophrenia have significantly different bacterial communities in their intestines.
The differences were so consistent that researchers could predict with surprising accuracy who had schizophrenia based solely on their gut bacteria profile, not their brain scans, not their symptoms, but their MICROBIOME.
But is this merely correlation? Here’s where science takes an extraordinary turn.
✅ From Correlation to Causation
To determine whether these microbes were actually CAUSING problems rather than just correlating with them, researchers conducted an experiment worthy of science fiction:
- They collected gut bacteria from people diagnosed with schizophrenia
- They transplanted these bacteria into germ-free mice (raised with no bacteria)
- They compared these mice to controls receiving bacteria from healthy humans
The results were stunning: Mice receiving the schizophrenia-associated bacteria developed behaviors remarkably similar to human schizophrenia symptoms, including reduced social interaction, cognitive impairments, and increased anxiety. Their brain chemistry showed alterations in glutamate and dopamine systems paralleling those in human schizophrenia.
Meanwhile, the control mice remained completely normal.
Let that sink in: the bacteria alone (without any genetic predisposition) were sufficient to trigger schizophrenia-like symptoms.
✅ GI Symptoms Precede Psychosis
Perhaps most telling: many schizophrenia patients report digestive problems years before their first psychotic episode. These weren’t random complaints. They may have been the earliest warning signs of disruption in the gut-brain axis.
ADHD: Reframing a “Brain Disorder” as a Gut Issue
ADHD affects approximately 5-7% of children and 2-5% of adults worldwide. We’ve attributed it to genetics, screen time, food additives, but the gut bacterial connection may be the critical missing piece.
❗ The ADHD Microbiome Is Distinctly Different
Multiple studies have identified consistent patterns in the gut bacteria of people with ADHD:
- Less Faecalibacterium (an anti-inflammatory bacterium)
- More Bacteroides (associated with Western diets and inflammation)
- Decreased Bifidobacterium (critical for gut barrier function)
- Reduced overall bacterial diversity (a hallmark of poor gut health)
These aren’t random variations. They appear consistently enough to suggest a fundamental biological connection between gut bacteria and ADHD symptoms.
❗ Gut Bacteria Directly Influence Dopamine
The connection to ADHD becomes even more compelling when we consider dopamine, the primary neurotransmitter targeted by most ADHD medications. Gut bacteria directly influence dopamine in several ways:
- Some bacteria produce dopamine themselves
- Others create precursors your body converts to dopamine
- Many affect how efficiently your body processes dopamine
- Some influence dopamine receptor sensitivity
A 2021 UC San Diego study found that mice with disrupted microbiomes showed reduced dopamine signaling in the prefrontal cortex, precisely the brain region critical for attention and executive function. When their microbiomes were restored with healthy bacteria, their dopamine function significantly improved.
This suggests a revolutionary possibility: what if some ADHD cases aren’t primarily brain disorders but rather neurological manifestations of an imbalanced gut ecosystem?
❗ The Antibiotic-ADHD Connection
One of the most compelling links comes from large population studies. A comprehensive Danish study of over 700,000 children found that antibiotic exposure before age 2 was associated with a 40% increased risk of ADHD diagnosis later in childhood.
Even more revealing: the risk increased with each additional course of antibiotics.
This makes perfect sense through a microbiome lens. Antibiotics don’t discriminate. They eliminate beneficial bacteria alongside harmful ones, potentially disrupting the gut-brain communication essential for attention and impulse control.
❗ Early Life: The Critical Window
For both gut bacteria and brain development, the first few years appear crucial:
- C-section delivery (which alters initial bacterial colonization) correlates with higher ADHD risk
- Formula feeding (vs. breastfeeding) affects both microbiome development and ADHD risk
- Early life stress disrupts gut bacterial development and increases ADHD risk
The patterns are too consistent to dismiss. The foundation for both your gut ecosystem and brain function is established during the same developmental window.
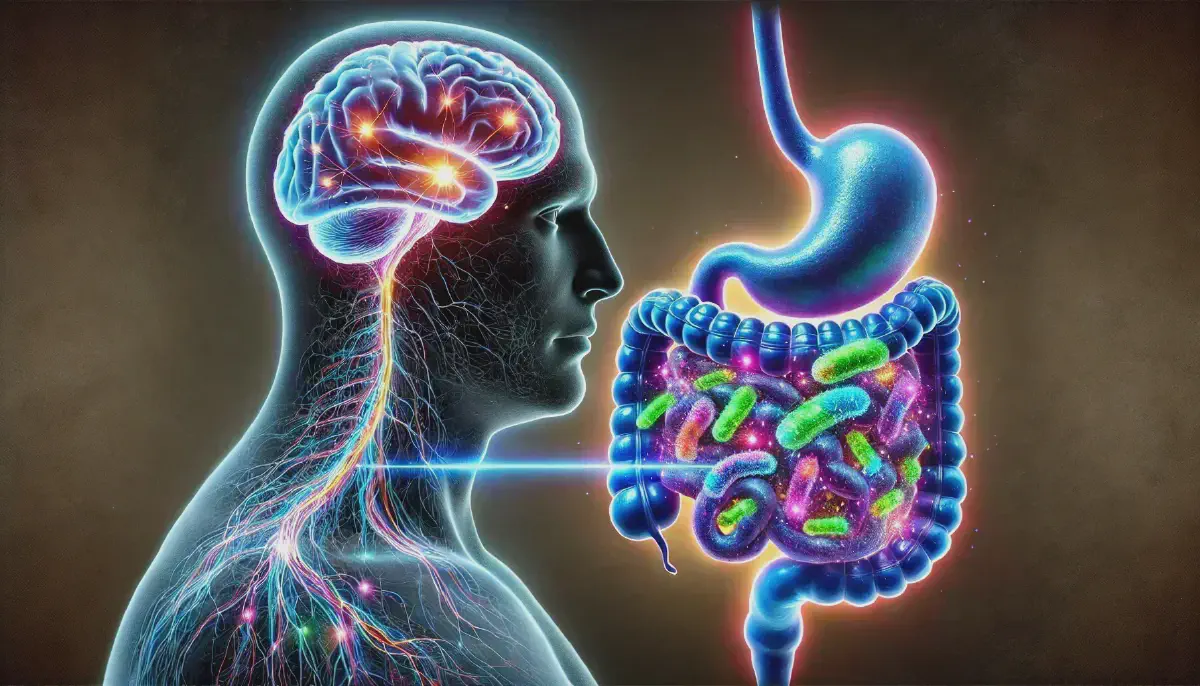
How Do Gut Bacteria Control Your Brain?
It sounds like science fiction, microscopic organisms in your intestines somehow manipulating your thoughts and behaviors. But the mechanisms are surprisingly direct:
1. The Information Highway: Your Vagus Nerve
The vagus nerve runs directly from your gut to your brain, carrying signals in both directions. Certain gut bacteria can activate this nerve, essentially sending direct messages to your brain. Some of these signals promote calm and focus, while others trigger anxiety and cognitive dysfunction.
2. Microbial Neurotransmitter Factories
Your gut bacteria produce neurotransmitters, the same chemicals your brain uses to function:
- GABA (the calming neurotransmitter)
- Serotonin (the mood regulator)
- Dopamine (the focus and motivation chemical)
- Norepinephrine (the alertness signal)
Remarkably, about 90% of your body’s serotonin is produced in your gut, not your brain. Your microbes are effectively operating a neurochemical factory in your intestines.
3. The Inflammation Connection
Both schizophrenia and ADHD have been linked to neuroinflammation, essentially the brain’s immune system in overdrive. What largely controls your body’s inflammatory responses? Your gut bacteria.
Some bacterial species trigger inflammation, while others suppress it. When pro-inflammatory species dominate, the resulting systemic inflammation can affect brain function, potentially contributing to symptoms of ADHD, schizophrenia, and other mental health conditions.
The Frontier: Poop Transplants and Designer Bacteria
This gut-brain connection has spawned treatments that would have seemed absurd (or just plain gross) a decade ago.
🔬 Fecal Microbiota Transplantation (FMT)
Fecal transplantation (transferring gut bacteria from a healthy donor to a patient) has evolved from fringe treatment to approved therapy for certain conditions.
For C. difficile infections, it boasts a 90% cure rate. Now, researchers are investigating FMT for mental health conditions, with early case reports showing promising results.
A 2022 case series documented five children with severe ADHD who received FMT for concurrent gut issues. Four showed “marked improvement” in ADHD symptoms following treatment.
🔬 Precision Bacterial Formulations
Scientists are developing precisely engineered bacterial combinations for specific conditions, not your average supermarket probiotics, but pharmaceutical-grade interventions targeting specific aspects of mental health.
For ADHD, research focuses on:
- Strains that regulate dopamine production
- Bacteria that reduce neuroinflammation
- Species that strengthen the gut barrier
Early clinical trials show promise. A 2021 double-blind placebo-controlled trial found that a specific multi-strain probiotic improved attention and reduced impulsivity in children with ADHD compared to placebo.
6 Ways to Fix Your Brain by Healing Your Gut
While research on targeted treatments advances, several evidence-based strategies can help restore microbial balance:
1. The 30 Plant Challenge
The strategy: Consume 30 different plant foods weekly. Each plant species provides unique compounds that nourish different bacterial populations.
This isn’t about endless salads. Herbs, spices, nuts, seeds, whole grains, fruits all count. Oregano, thyme, and rosemary? That’s three different plants already.
The landmark American Gut Project found that people who ate 30+ plant foods weekly had significantly more diverse microbiomes than those who ate fewer than 10.
2. Fiber Diversity Is Key
Different types of fiber feed different bacterial communities:
- Soluble fiber (oats, beans, apples)
- Insoluble fiber (whole grains, vegetable skins)
- Resistant starch (cooled potatoes, green bananas, legumes)
- Prebiotic fibers (onions, garlic, leeks, Jerusalem artichokes)
Start gradually if your current diet is low in fiber. Too much too soon can cause uncomfortable gas and bloating as your microbiome adapts.
3. Embrace Fermented Foods
A 2021 Stanford study found that consuming six servings of fermented foods daily increased microbiome diversity more effectively than even a high-fiber diet. Include:
- Yogurt with live cultures
- Kefir (dairy or water-based)
- Unpasteurized sauerkraut and kimchi
- Traditionally fermented pickles (refrigerated, not shelf-stable)
- Miso, tempeh, and natto
The key is looking for products with live cultures that haven’t been heat-treated after fermentation.
4. Eliminate the Chemical Feast
Ultra-processed foods, artificial sweeteners, and food additives can disrupt your gut ecosystem:
- Emulsifiers (like carboxymethylcellulose and polysorbate-80) damage the protective mucus layer in your gut
- Artificial sweeteners alter bacterial metabolism in ways that affect brain function
- Preservatives can selectively kill beneficial bacteria while allowing harmful ones to thrive
A 2020 study found that switching participants to an ultra-processed diet for just two weeks reduced gut microbial diversity by 30%. TWO WEEKS.
5. Rethink Antibiotics (When Appropriate)
Antibiotics are sometimes necessary and lifesaving. But they’re also massively overprescribed, especially for viral infections where they do nothing but destroy your gut bacteria.
If you do need antibiotics:
- Ask if a narrow-spectrum (rather than broad-spectrum) antibiotic would suffice
- Complete the full course as prescribed
- Consider probiotic supplementation during and after
- Increase prebiotic-rich foods to help beneficial bacteria recover
6. Break the Stress-Gut Cycle
Chronic stress disrupts your gut bacteria, which then produce fewer calming compounds, which makes you more susceptible to stress… and the vicious cycle continues.
Practices that reduce stress (meditation, adequate sleep, time in nature, exercise) directly benefit your microbiome’s health and composition.
The Bottom Line: A Mental Health Revolution
The gut-brain connection isn’t just another health trend. It represents a fundamental shift in how we understand disorders like schizophrenia and ADHD. We’re transitioning from a brain-centered model to one that recognizes the profound influence of the gut ecosystem on mental function.
This perspective changes everything:
- Mental health conditions might be partially treated through the gut
- Neurodevelopmental disorders might be influenced by early microbiome interventions
- The artificial boundary between “mental” and “physical” health requires rethinking
Will this approach replace traditional medications overnight? Of course not. But it opens new avenues for complementary approaches that might enhance existing treatments or help people who don’t respond well to conventional therapies.
The microbiome revolution offers something that’s been scarce in mental health treatment: hope based on a new paradigm, not just refinements to an existing one.
Your gut bacteria aren’t just passive passengers. They’re active participants in your mental health. And finally, we’re beginning to listen to what they’ve been telling us all along.